
When lives depend on rapid, scarce resources and equipment it makes sense to get the best minds looking into diverse solutions, including those tried and tested that have proved successful in the past.
The iron lung saved thousands of lives of polio victims around the world in the twentieth century, and has the potential to do the same to those infected by Covid-19 in the current global pandemic.
Leading engineers from Marshall Aerospace and Defence Group have been working together with British citizen scientists, medical clinicians, academics, manufacturers and engineers to develop an alternative model of ventilator to support the Government’s drive to equip the NHS.
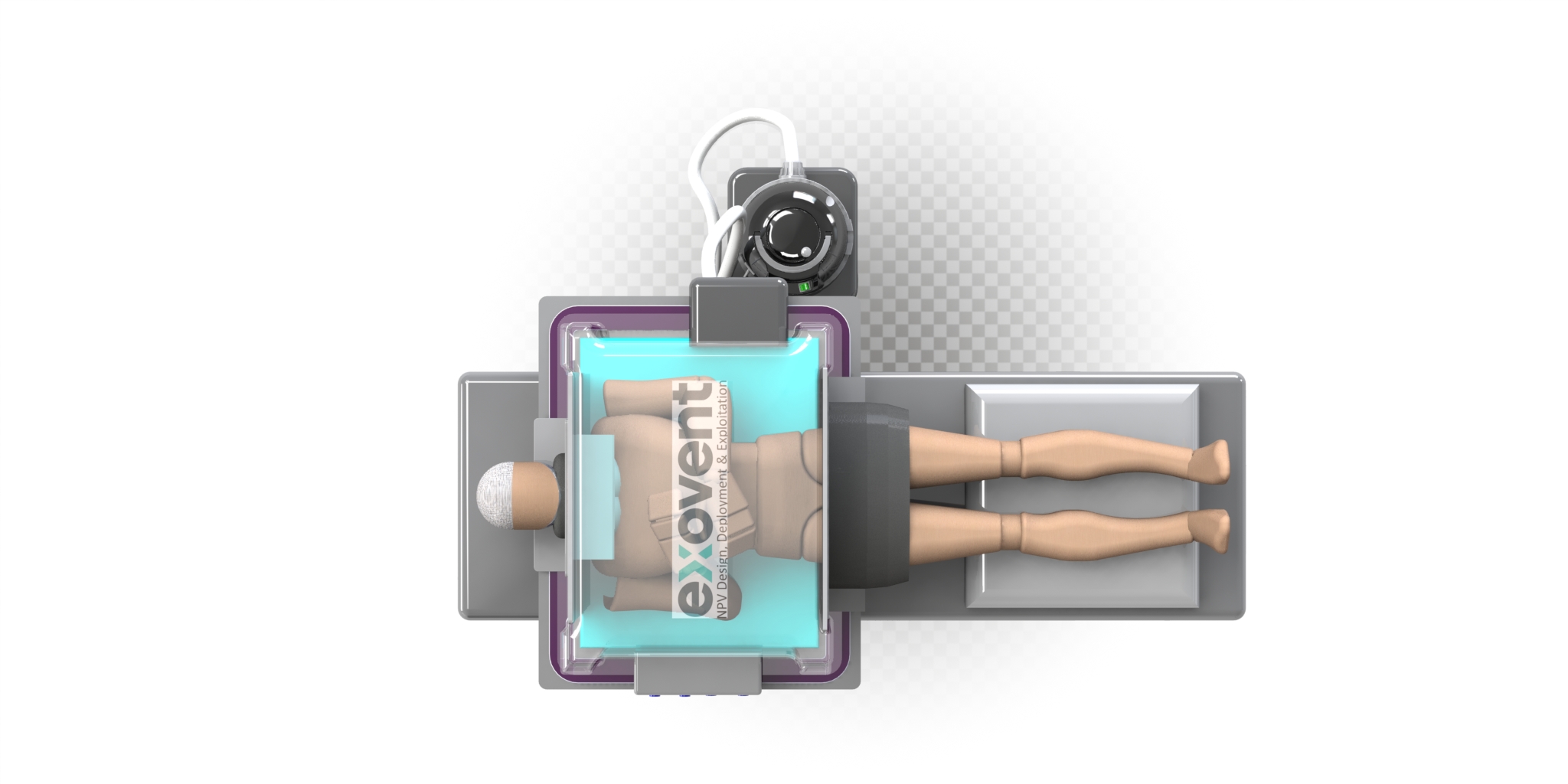
The new model, the Exovent, is a cutting-edge reinvention of the archetypal iron lung, a Negative Pressure Ventilator (NPV), which is non-invasive and allows the patient to remain conscious throughout treatment.
Conventional, modern Intermittent Positive Pressure Ventilators (IPPV) require the patient to be intubated via their windpipes, which means they have to be sedated, and sometimes even paralysed, while their chest is squeezed to introduce and remove air into their lungs.
The NPV, on the other hand, does not require this invasive procedure, but instead patients remain conscious, can take medications and food by mouth instead of drip, and continue to be able to speak.
Exovent also increases the heart’s efficiency by up to 25 per cent compared to conventional ventilators, which may actually reduce cardiac function, and further deteriorate a patient’s already compromised cardiac function.
It has the added advantage of being easy to use and able to be located on a normal ward. This keeps patients out of intensive care and so frees up those valuable facilities and ICU clinicians for the most serious cases.
Patients can be easily treated and monitored, can lie on their fronts, which is an effective treatment for pneumonia, and are less likely to experience micro trauma to the lungs.
Marshall ADG Chief Technical Officer, Patrick Wood said:
“This is one of a number of projects we are involved in following the government’s call to industry for support in the battle against Covid-19 and we are incredibly proud that our engineering talent is being put to such important use,”
Exovent does not require compressed air or oxygen to operate and provide excellent oxygen and carbon dioxide transfer.
NPVs can be rapidly manufactured using only a small number of moving parts, which are currently readily available in the UK and not required by other manufacturers working to build conventional ventilators for Government.
This means that round 5,000 NPVs can be produced every week, and adapted to provide clinicians with options to choose the most appropriate devise to treat individual patients.
“Clearly there is still long way to go but I am very excited about the potential of the Exovent product. It has so many positive attributes in terms of cost, ease of production and application, and at the same time doesn’t use any of the same parts that are being used in the production of the much needed positive pressure ventilators,”
said Patrick.
The Exovent concept is also supported by WMG at the University of Warwick and representatives from Imperial NHS Trust and The Royal National Throat Nose and Ear hospital. Two leading intensive care units have agreed to trial the prototype ventilator support devices.
Image source: John Hunter, Steer Energy